Seniors aged 65 years and over account for the highest number of patients in the emergency department (ED) in the United States. While older adults visit the ED due to age-related challenges, abdominal pain is the most common presenting complaint. According to researchers, elderly patients tend to suffer from more complex abdominal problems, which are difficult to diagnose. Older adults are at a higher risk of frequent and severe stomach infections and inflammation due to weaker levels of immunity. Also, an aging GI (Glycemic Index) system leads to decreased emptying time and fundal compliance. Therefore, it can eventually lead to acid reflux and digestive disorders.
Besides, both the central and peripheral nervous systems of the brain are also affected by aging. Due to the prevalence of dementia and cognitive impairment, seniors can also suffer from atypical abdominal pain. Here are a few common reasons for stomach aches in the elderly.
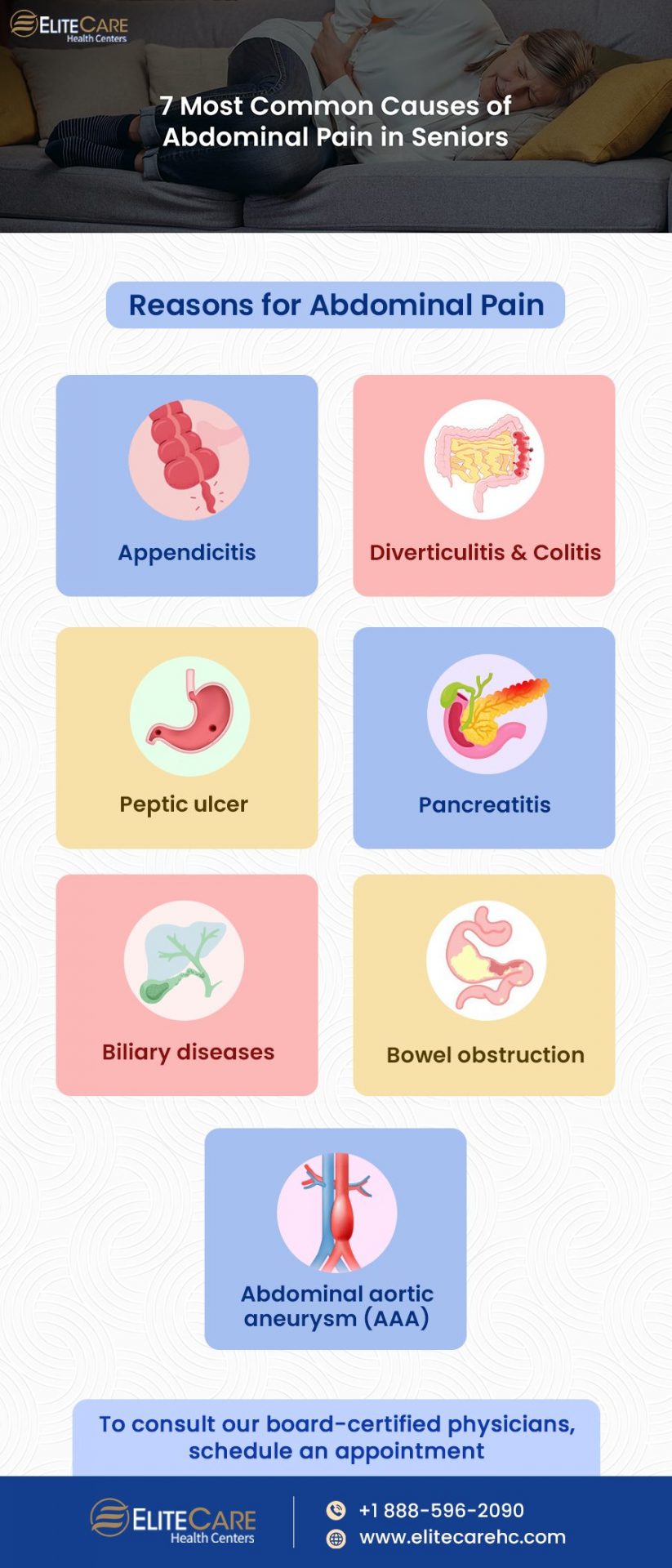
Reasons for Abdominal Pain
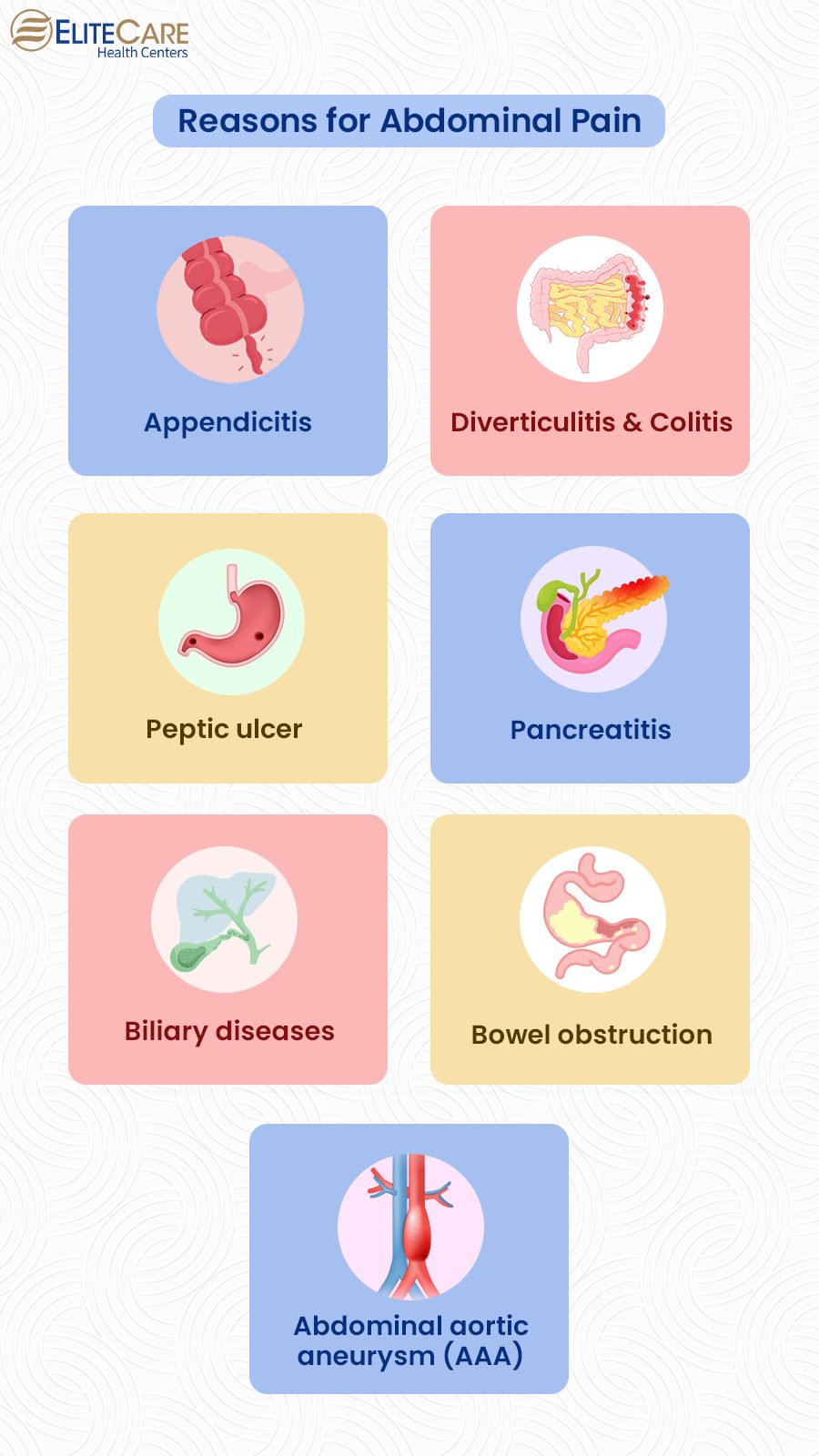
1. Appendicitis
Appendicitis is a diagnostic challenge for patients of all ages, but it can be even more difficult for older adults. Appendicitis pain is generally localized to the right lower quadrant and it has additional symptoms such as nausea and vomiting. No laboratory test can reliably diagnose appendicitis in the elderly, but the recent use of C-reactive protein lab test for this purpose has been promising. However, definitive imaging or laparotomy is still required to diagnose appendicitis.
Read More: Can Certain Food Improve Your Brain Health?
2. Diverticulitis and Colitis
Aging and lifestyle changes place the elderly at high risk for constipation, colitis, and diverticulitis. Diverticulitis classically presents as left lower abdominal pain and cramping. It also shows additional symptoms like changes in bowel movements, nausea, or fever. Generally, diverticulitis is diagnosed by contrast-enhanced CT because it can rule out alternative diagnoses that may not be well visualized by other imaging modalities. Initial treatment of this abdominal problem consists of broad-spectrum antibiotics against gram-negative and anaerobic bacteria, with a typical course that lasts 7 to 10 days.
Colitis shows similar symptoms to diverticulitis and is caused by infectious agents, such as Clostridium difficile, and inflammatory bowel disorders, such as ulcerative colitis (UC) and Crohn’s disease. Stool antigen analysis, CT scan, and colonoscopy may help identify the causes of this colonic inflammation.
3. Peptic ulcer
Researchers reveal that peptic ulcer disease accounts for 16 percent of older patients complaining of abdominal pain. For the past few years, hospital admission rates for PUD-related complications have increased in older adults, mainly because of the increased use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs). These increase the risk of developing gastroduodenal injury in the elderly. The symptoms of peptic ulcer disease are usually absent or poorly localized as most seniors suffering from ulcers don’t suffer from any kind of abdominal pain. While plain film abdominal radiographs are helpful in some cases, Barium contrast studies and upper endoscopy can confirm the diagnosis of peptic ulcer more easily.
4. Pancreatitis
The most common nonsurgical cause of abdominal pain among older adults is pancreatitis. Usually, seniors suffer from upper abdominal pain that eventually radiates to the back. But in some cases, it can also present as diffused abdominal, back, or chest pain, along with nausea and vomiting. The most common reasons behind acute pancreatitis in older patients are alcoholism, biliary tract disease, infections, hypertriglyceridemia, a variety of medications, hypercalcemia, hypothermia, and exposure to carbon monoxide.
Imaging is particularly helpful in patients with atypical presentations. For gallstone pancreatitis, Endoscopic retrograde cholangiopancreatography (ERCP) is the recommended therapeutic and diagnostic test. It is crucial to diagnose pancreatitis early to reduce risk factors such as organ dysfunction, systemic inflammatory response syndrome, or even death.
5. Biliary diseases
In the geriatric population, biliary tract disorders are the most common cause of abdominal pain and the most common indication for intra-thoracic surgery. The risk of gallstones increases with age as bile acid production, bile cholesterol saturation, and gallbladder sensitivity change as well. Gallstones only show symptoms when they obstruct the neck of the gall bladder, resulting in abdominal pain, often accompanied by anorexia, nausea, and vomiting. Symptomatic cholelithiasis is treated with elective cholecystectomy if the pain is moderate.
Early surgical intervention can reduce the risk of severe complications, including obstructive jaundice, acute cholecystitis (AC), pancreatitis, cholangitis, perforation, and empyema. While ERCP is the most commonly used diagnostic procedure, magnetic resonance cholangiopancreatography and endoscopic U/S are now given more importance because they are less invasive.
6. Bowel obstruction
The small bowel is the most common site of obstruction as it is narrower in diameter. Older adults with small bowel obstruction suffer from frequent abdominal pain, nausea, vomiting, abdominal distension, and constipation.
While plain radiography is often the initial study of choice, it is limited to the assessment of the degree, location, and cause of obstruction. CT imaging should be obtained when radiographs cannot clearly discriminate between complicated (vascular involvement) and uncomplicated (bowel involvement only) obstruction.
7. Abdominal aortic aneurysm
An abdominal aortic aneurysm (AAA) usually originates in the infrarenal arteries and extends into the iliac arteries. Older adults who have a history of using tobacco are at the highest risk for AAA as smoking is the strongest independent risk factor for this disease.
Often, AAA is asymptomatic and even when symptoms develop, they are usually nonspecific in nature. It can cause abdominal pain, backache, or claudication. But if ruptured, AAA causes severe abdominal pain, back or flank pain, hypotension, and a pulsatile mass on examination. While plain radiographs can only show calcifications of the aneurysm, a soft tissue mass, loss of the psoas shadow, or loss of renal outline, ultrasonography is a faster, safer, and more reliable way to distinguish an abdominal aneurysm.
Read More: Seniors: Are you drinking enough water?
Key Takeaway
Abdominal pain in older adults is a concerning symptom common to a variety of diagnoses with high chances of morbidity and mortality. Therefore, it is crucial to be mindful of the signs and take the patient to the hospital, co and consult the doctor at the earliest to avoid further risks. To receive the best primary care services in Florida, Contact EliteCare Health Centers and schedule an appointment.
Frequently Asked Questions
Abdominal pain in the elderly can stem from various causes, including gastrointestinal issues like diverticulitis or peptic ulcers, urinary tract infections, or even heart problems like angina. Identifying the source often requires medical evaluation due to the diverse range of potential issues.
Signs of pain in the elderly might include altered behavior like agitation or withdrawal, changes in eating or sleeping patterns, and non-verbal cues like grimacing, guarding certain body areas, or reduced mobility. Identifying these signs can help in addressing and managing pain effectively in older individuals.
To manage pain in older age, options include over-the-counter pain relievers like acetaminophen or NSAIDs (under doctor’s guidance), physical therapy or gentle exercise to improve mobility and strength, and complementary approaches such as acupuncture or heat/cold therapy, all under supervision to ensure safety and efficacy.
There are three main types of abdominal pain: visceral, parietal, and referred pain. Visceral pain happens when the nerves that run through the walls of an organ get stretched. The pain isn’t usually well localized and feels like a dull ache or cramp.