Diabetes is a chronic condition that affects the body in multifaceted ways. The eye is one of the most vulnerable and often overlooked targets of diabetes. According to studies, diabetes is one of the leading causes of blindness among adults aged 18 to 64 years in the United States.
Diabetic retinopathy is one of the most reported vision-related problems individuals with diabetes suffer from. It can significantly affect vision and lead to blindness if not addressed on time. In this blog post, we will share detailed insights into diabetic retinopathy symptoms, causes, effects, types, treatments, and preventive measures. Read on to learn more.
What is Diabetic Retinopathy?
Diabetic retinopathy is a progressive eye condition that arises as a long-term complication of uncontrolled diabetes. It specifically affects the retina, the light-sensitive tissue lining the back of the eye that transmits visual signals to the brain. When left untreated, diabetic retinopathy can lead to severe vision impairment and even permanent blindness.
If not addressed for an extended period, high blood sugar levels can damage small blood vessels that nourish the retina, also known as retinal blood vessels. These blood vessels may gradually start leaking or get blocked, impairing the blood flow to the retina and eventually forming scar tissue on the retina.
The longer a person is suffering from diabetes, the higher the risk of developing diabetic retinopathy. Additionally, high blood pressure levels, high cholesterol levels, and other pre-existing conditions such as kidney disease or anemia may heighten the risk of diabetic retinopathy.
Types of Diabetic Retinopathy
1. Non-Proliferative Diabetic Retinopathy (NPDR)
This is the early stage of Diabetic Retinopathy, often referred to as background retinopathy as well. At this stage, the retinal blood vessels begin to show signs of damage due to the consistent impact of elevated blood sugar levels. There are two subcategories within NPDR, which are as follows:
a. Mild NPDR
In mild NPDR, small areas of the retinal blood vessels weaken and may leak tiny amounts of fluid or blood into the retina. These microaneurysms may not cause immediate vision problems, but they indicate the need for proper medical intervention to prevent progression.
b. Moderate NPDR
As NPDR advances to a moderate stage, the retinal blood vessels become more damaged. This may include increased swelling or vessel blockage, leading to restricted blood flow and low vision.
2. Proliferative Diabetic Retinopathy
This is an advanced stage that can potentially lead to complete vision loss. PDR involves the proliferation or growth of new and abnormal blood vessels on the surface of the retina. These new vessels are fragile and prone to leakage, leading to the formation of scar tissue and exacerbating the existing vision-related problems.
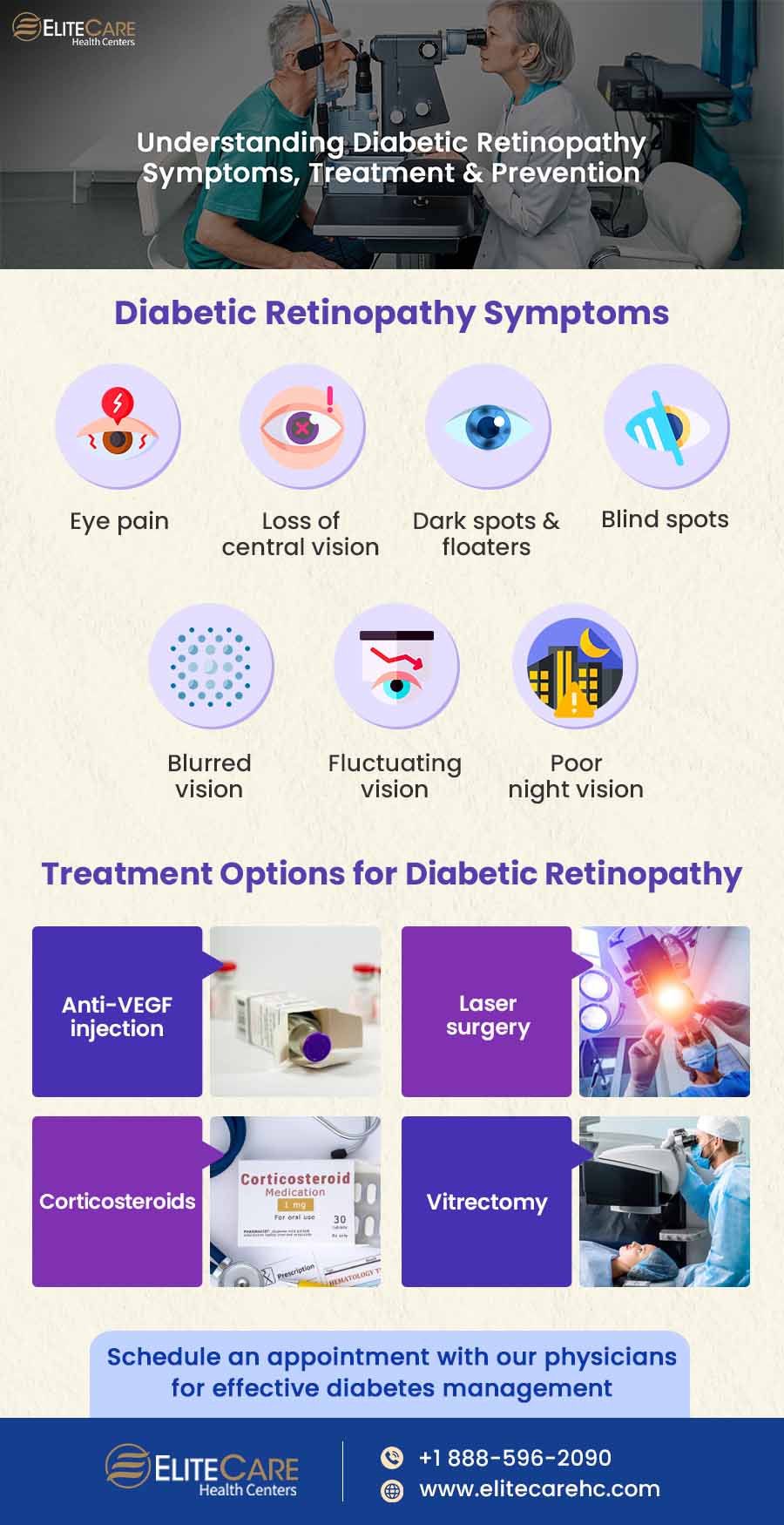
Diabetic Retinopathy Symptoms
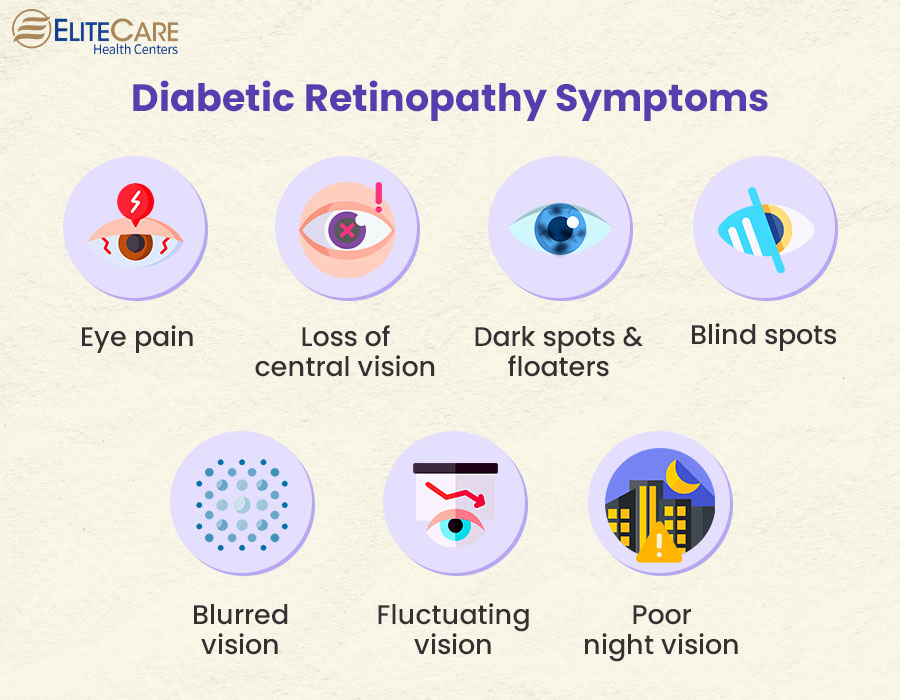
At an early stage, diabetic retinopathy doesn’t usually cause any significant symptoms, except for some visual discomfort. In the moderate to more advanced stage, it may produce the following symptoms:
- Eye pain
- Loss of central vision, especially experienced during reading or driving
- Dark spots or strings floating in your vision (floaters)
- Blind spots
- Blurred vision
- Fluctuating vision
- Poor night vision
Diabetic retinopathy usually affects both eyes, and individuals may notice its symptoms in one eye at the beginning. While some individuals may only experience poor vision, others may experience multiple symptoms. It is crucial to consult a primary care physician immediately for any concerns.
What Are the Other Complications That May Arise From Diabetic Retinopathy?
1. Diabetic Macular Edema (DME)
It is a critical complication that occurs when the damaged blood vessels of the retina leak fluid into the macula, the central and most sensitive part of the retina. This accumulated fluid causes swelling in the macula and eventually results in blurred or distorted central vision. Individuals experiencing DME may find it challenging to read, drive, or recognize faces.
2. Neovascular Glaucoma
In cases of Proliferative Diabetic Retinopathy (PDR), the growth of abnormal blood vessels in the iris can obstruct the eye’s drainage system. It can increase intraocular pressure, leading to neovascular glaucoma, which can cause severe eye pain, vision loss, and even irreversible damage to the optic nerve.
3. Retinal Detachment
The formation of scar tissue in the retina due to the growth of abnormal blood vessels can lead to retinal detachment. When scar tissue contracts, it causes the retina to lift or detach from its normal position.
4. Vitreous Hemorrhage
As the disease progresses, the fragile abnormal blood vessels can rupture and bleed into the vitreous, a gel-like substance that fills the center of the eye. Vitreous hemorrhage can cause sudden and dramatic vision loss.
How is Diabetic Retinopathy Treated?

1. Anti-VEGF Injection Therapy
This treatment procedure has revolutionized the outlook for Diabetic Retinopathy, particularly in cases of Diabetic Macular Edema (DME) and Proliferative Diabetic Retinopathy (PDR).
VEGF, a protein, stimulates the growth of abnormal blood vessels in the eye and contributes to the progression of the disease. Injecting anti-VEGF drugs directly into the eye can inhibit VEGF activity, and therefore reduce leakage from abnormal blood vessels. It can help prevent more severe complications like neovascular glaucoma and vitreous hemorrhage.
2. Laser Surgery (Photocoagulation)
Healthcare professionals recommend laser photocoagulation treatment for diabetic retinopathy, primarily to manage Proliferative Diabetic Retinopathy (PDR) and some cases of Diabetic Macular Edema (DME).
In this procedure, a focused laser beam is applied to the retina to prevent leakage from blood vessels and induce controlled scar tissue formation. This process helps reduce the abnormal growth of fragile blood vessels and stabilize the retina, preventing further complications like retinal detachment.
3. Corticosteroids
In cases of Diabetic Macular Edema (DME) and certain forms of Non-Proliferative Diabetic Retinopathy (NPDR), healthcare professionals may use corticosteroids to reduce inflammation and fluid buildup in the retina. These steroids can be either delivered through injections or as implants within the eye to prevent macular edema and improve vision.
However, the effects of corticosteroids may be temporary, and long-term use can carry potential risks, such as increased eye pressure.
4. Vitrectomy
This is a surgical procedure that physicians typically recommend for managing severe complications, such as vitreous hemorrhage and retinal detachment. During vitrectomy, the surgeons remove the vitreous gel from the eye and replace it with a clear solution. This procedure helps restore clear vision and facilitate better access to the retina. Vitrectomy may also involve removing scar tissue or treating retinal tears and detachments.
The choice of treatment depends on various factors, including the stage of Diabetic Retinopathy, the presence of complications, and the individual’s overall eye health. In many cases, a combination of treatments might be recommended to achieve the best possible outcomes. Visit a medical clinic and consult a primary care physician or ophthalmologist for detailed guidance.
Can Diabetic Individuals Prevent Diabetic Retinopathy?
While certain risk factors may be beyond our control, individuals suffering from diabetes can take a few measures to reduce the risk of Diabetic Retinopathy. The following are some crucial steps that can make a significant difference:
- Take medication or insulin as prescribed by healthcare professionals.
- Monitor blood sugar levels at regular intervals and consult a physician if high glucose levels persist over an extended period.
- Get comprehensive eye check-ups at least once annually, or more frequently as recommended by an eye care specialist.
- Keep blood pressure and cholesterol levels under control, which can further exacerbate retinal blood vessel damage.
- Quit smoking, which can particularly damage blood vessels throughout the body, including those in the retina.
The Bottom Line
According to the Centers for Disease Control and Prevention, approximately one in four adults with diabetes in the US has Diabetic Retinopathy. Although it is not entirely preventable, adequate knowledge and information about this disease can help us take proactive steps to reduce our risks. Additionally, early diagnosis can improve treatment outcomes and reduce the risk of partial or complete blindness. Do not miss regular eye check-ups and convey any concerns to the primary care physician or ophthalmologist promptly to receive an accurate diagnosis and timely treatment.
For any queries or concerns about Diabetic Retinopathy in seniors, contact EliteCare Health Centers, one of the best healthcare centers and senior care service providers in Florida, offering a wide range of primary care services.